
How to Integrate AI with PACS and RIS Systems?
Integrating “AI into PACS” and RIS workflows is a crucial step that transforms advanced AI algorithms into practical tools for radiology. Because PACS is the key operating environment for radiologists, the main challenge is not adopting AI but rather embedding it into everyday workflows so that radiologists can work faster, make confident decisions, and deliver better patient care.
Radiology departments stand to gain significantly from AI solutions that automate repetitive tasks, prioritize urgent studies, and populate structured reporting measurements. However, integration demands careful planning around interoperability standards like DICOM and FHIR, infrastructure readiness, and regulatory compliance. RamSoft’s cloud-native, API-first architecture is designed precisely to meet these requirements, enabling seamless connections to AI tools from multiple vendors while maintaining security and efficiency.
This guide explores the key steps and challenges of integrating AI within PACS and RIS systems. It covers why AI integration matters for modern radiology, the different connection models available, common workflow and technical barriers, and proven strategies to ensure successful deployment. We also examine how RamSoft’s cloud-native architecture supports seamless, secure AI integrations and looks ahead to emerging trends shaping the future of AI in radiology.
- AI integration in PACS and RIS streamlines workflows, reduces repetitive tasks, and supports consistent diagnostic accuracy.
- Both native and bolt-on approaches have value: native offers seamless user experiences, while bolt-on provides flexibility to use specialized tools.
- Cloud-based, API-driven systems make AI deployment scalable, secure, and easier to maintain.
- Real-time prioritization of urgent cases improves turnaround times, helping radiologists deliver faster, higher-quality patient care.
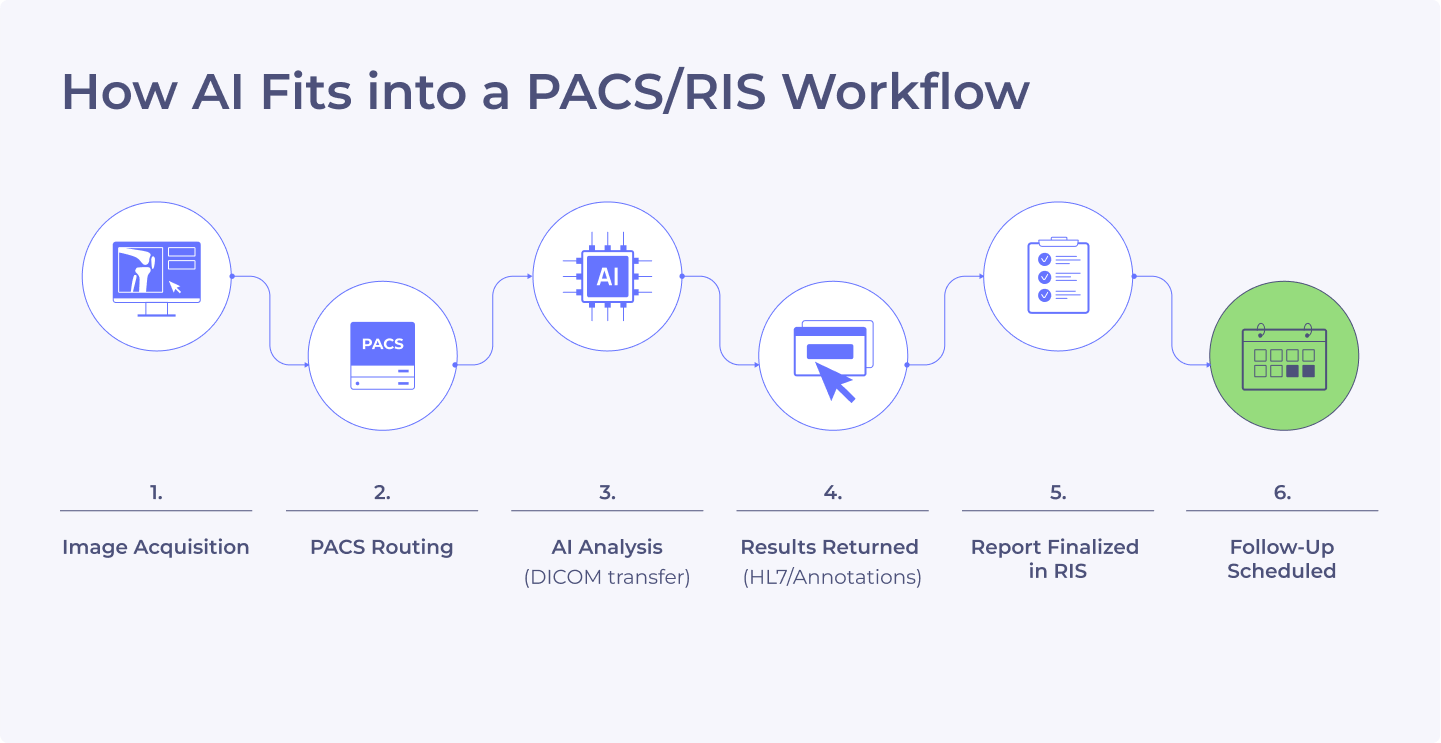
How AI Connects to Your Existing PACS/RIS Workflow?
AI integration with PACS and RIS systems is about choosing the right connection model that fits both clinical and IT needs. AI tools can be embedded directly into imaging platforms (native integration) or connected as external applications (bolt-on). Understanding these models is key to determining how AI insights flow into radiology workflows, how studies are routed between systems, and how automated triggers operate. The following sections explain these approaches and their impact on workflow efficiency, IT overhead, and scalability.
Native Integration vs. Bolt-On AI Workflows
AI can be connected to PACS and RIS through native integration or bolt-on solutions, each offering specific advantages.
Native integration places AI tools directly inside the PACS or RIS interface. Examples include iCAD, AlphaNodus, NewVue, and Therapixel, which are embedded within PowerServer™ so radiologists can view AI results alongside images without leaving their primary viewer. This approach improves workflow efficiency, reduces clicks, and makes AI insights available instantly.
Bolt-on integrations connect external applications that operate separately from PACS or RIS, such as cardiology structured reporting. These tools may run on dedicated platforms but are linked to the imaging workflow through DICOM routing, HL7 messaging, or other integration methods. Bolt-on solutions allow radiology practices to add specialized capabilities without replacing existing systems.
Both approaches are valuable. Native integrations offer seamless user experiences, while bolt-on solutions provide flexibility to add targeted functionality as needs evolve.
Push vs. Pull Integration Models
Most AI workflows use a push model, where studies that match defined rules are automatically routed from PACS or RIS to the AI engine via DICOM. The AI analysis is then returned, often as annotations or structured reports, through HL7 messaging. This setup reduces manual steps and ensures results are available as soon as radiologists open the study.
Pull models, where the AI system queries PACS for studies, are less common due to increased complexity and slower response times. RamSoft systems are optimized for push-based workflows, enabling smooth and reliable data exchange between PACS, RIS, and AI engines.
Automating AI Triggers Based on Study Attributes
Automation improves consistency and eliminates unnecessary manual work. PACS and RIS can automatically send studies for AI analysis when they meet predefined rules based on modality, body part, or clinical indication. For example, Therapixel can automatically process all mammography exams, including prior mammography exam images, to detect and highlight anomalies or changes before radiologists review them.
Similarly, AI-CAD solutions can assign a score to each pre-analyzed study, with higher scores automatically prioritized in the worklist to ensure urgent cases are read first. This type of automation ensures AI is applied uniformly, reduces the chance of missed findings, and allows radiologists to start with pre-analyzed studies. In high-volume imaging practices, automated triggers save time and reduce workflow bottlenecks.
Improving Radiology Workflow Efficiency with AI
AI improves workflow efficiency by handling repetitive tasks such as measurements, annotations, and preliminary case triage. Radiologists receive studies that have already been analyzed, complete with highlighted areas of concern, structured data, and probability scores.
iCAD’s AI for mammography is an example of how pre-analyzed studies accelerate review times. Radiologists can adjust AI-generated insights instead of performing every measurement manually, which shortens turnaround times and reduces cognitive fatigue.
By reducing manual work and providing decision support, AI helps radiologists focus on complex cases and patient outcomes rather than administrative tasks. Over time, this leads to faster reporting, fewer errors, and higher overall efficiency.
Why Integrate AI with PACS and RIS?
For radiology practices working to keep pace with rising imaging volumes and increasing demands for precision care, integrating AI into PACS and RIS systems is now a strategic priority. The value lies not only in embedding AI into a single interface, but in making AI insights accessible within the radiologist’s routine clinical workflow using flexible integration models, including bolt-on solutions.
RamSoft’s standards-based architecture supports this flexibility by delivering AI results directly into clinical workflows without unnecessary complexity. This allows practices to move from reactive decision-making to proactive, data-driven operations that improve speed, accuracy, and consistency. In critical use cases such as intracranial hemorrhage detection, AI-enabled triage has reduced diagnostic times by up to 90 percent, helping radiologists act faster and improving patient outcomes.
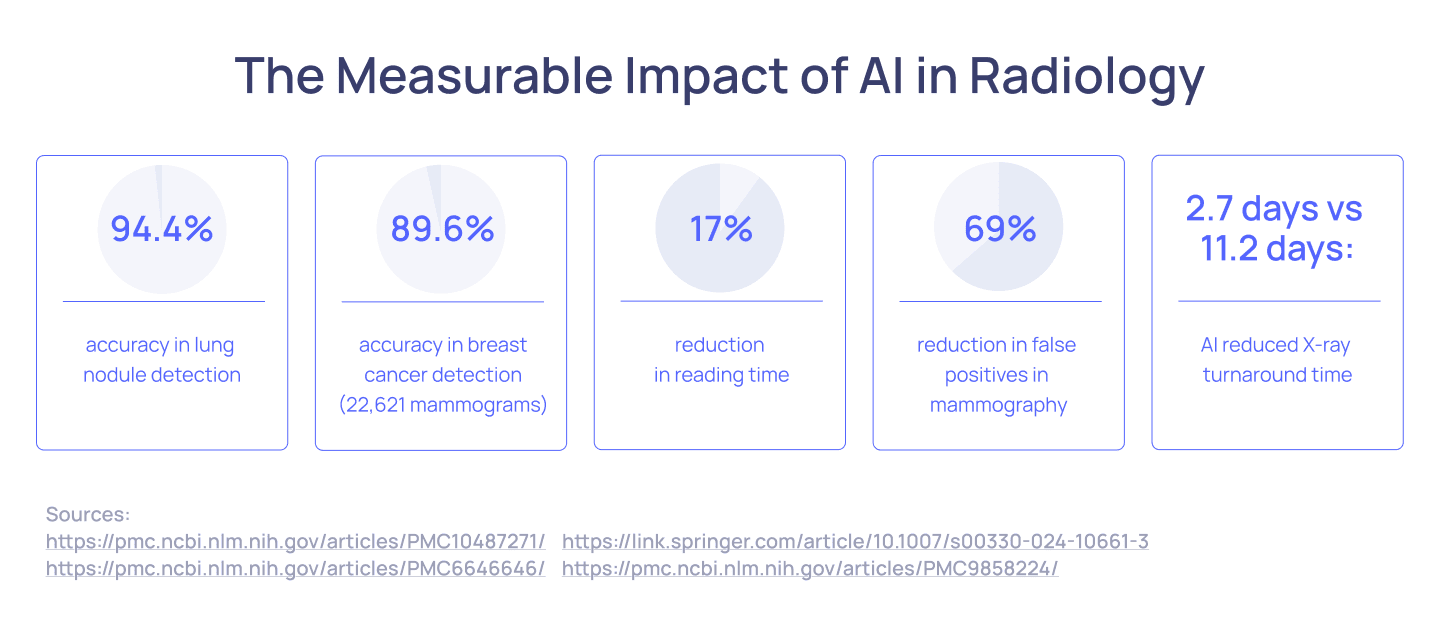
Accelerates Turnaround Times
Speed is crucial in radiology for both patient care and operational efficiency. Integrating AI into PACS shortens the time from image acquisition to reporting by automating repetitive tasks and enhancing reading speed. AI-powered solutions rapidly analyze imaging data, delivering preliminary insights that help radiologists focus on high-priority findings instead of manual processes.
AI drives faster workflows in several ways. It can measure lesions, segment organs, and compare current exams with prior studies. In one study by Annarumma et al., an AI triage tool reduced the reporting delay turnaround time for critical chest X-rays from 11.2 days to 2.7 days, showing how AI can greatly accelerate case prioritization in high-volume settings.
Embedding AI results directly into PACS viewers lets radiologists view annotations and alerts alongside images without toggling between systems. This seamless integration eliminates extra steps, saving time across busy departments and enabling quicker decisions for referring physicians, ultimately improving patient outcomes.
Prioritizes Critical Cases in Real Time
Integrating AI into RIS enables real-time reprioritization of cases based on clinical urgency, ensuring radiologists focus attention where it matters most. For instance, if AI detects a chest CT suspicious for pulmonary embolism, the study can automatically move higher on the worklist with color-coded alerts, prompting immediate review ahead of routine cases.
This dynamic triage replaces the traditional “first in, first read” approach, preventing delays and reducing the manual effort required to reorder cases. Hospitals can set customizable rules so that priorities reflect the severity of findings, local health needs, staffing, or resource availability. Radiologists see these updates directly in their RIS dashboards, preserving familiar workflows while improving responsiveness.
Reduces Manual and Repetitive Tasks
Radiologists handle many repetitive tasks daily, such as lesion measurements, organ segmentation, and follow-up comparisons, all essential for precise reporting but time-consuming and mentally draining. Integrating AI into PACS and RIS automates these processes, easing radiologists’ workload and improving efficiency.
AI tools can automatically segment and measure tumors for oncology imaging, label anatomical structures across modalities, identify and insert guidelines, and compare current studies to prior exams to identify interval changes. This automation accelerates report creation and reduces cognitive fatigue, allowing radiologists to concentrate on complex diagnostic decisions rather than routine measurements.
Moreover, AI standardizes repetitive tasks, enhancing consistency across different radiologists and shifts. In high-volume practices, this uniformity is crucial for maintaining quality and compliance with evidence-based guidelines. AI also helps automate follow-up recommendations, ensuring patients receive timely care while reducing administrative burdens tied to managing recalls and future imaging schedules.
Enhances Diagnostic Accuracy and Consistency
Diagnostic accuracy defines radiology’s value to patient care, yet interpretations can vary due to fatigue, complexity, or subtle findings. AI serves as a consistent second reader, scanning thousands of images rapidly to detect patterns often imperceptible to human eyes.
AI systems have achieved notable performance, such as YOLO-based models reaching up to 98.7% accuracy in lung cancer detection on CT scans. In breast imaging, AI-assisted interpretation has reduced false positives by 37.3% and unnecessary biopsies by 27.8%, while identifying up to 49.8% of interval cancers missed by radiologists, underscoring its role in early disease detection and consistent reporting.
Beyond single cases, AI helps standardize readings across radiologists, supporting quality assurance and compliance. It also serves as an educational tool, enabling radiologists at all experience levels to refine diagnostic skills and fostering continuous learning within imaging teams.
Improves Reporting and Structured Data Capture
Accurate and consistent reporting is essential for radiology’s impact on patient care and broader healthcare analytics. Traditional narrative reports often differ in structure and detail, making it difficult to support data-driven decision-making, coding accuracy, and seamless integration with electronic health records (EHRs).
Integrated AI tools within RIS and reporting systems address these gaps by automatically populating structured templates, extracting key clinical data for registries or research, and generating standardized language to reduce ambiguity. For example, an AI system identifying a 5mm lung nodule can measure it, insert the finding into a structured report, and provide follow-up recommendations based on Fleischner guidelines all without manual effort.
Structured reporting improves data quality and enables advanced analytics, supporting interoperability through standards like FHIR and DICOM SR. By embedding AI into reporting workflows, radiology practices transition from purely diagnostic services to data hubs that generate insights for enhancing patient care and operational efficiency across the healthcare system.
Workflow Challenges in AI Integration
Adopting AI in radiology promises significant benefits, but the path to integration isn’t without obstacles. Radiology practices must navigate operational challenges that can impact everything from IT infrastructure to clinical workflows and regulatory compliance.
Equally crucial is selecting the right vendor. This partner should go beyond simply providing technology, offering guidance for full implementation, ensuring interoperability, and supporting ongoing optimization.
RamSoft exemplifies this role with its cloud-native platforms and deep expertise, helping practices integrate AI seamlessly into daily operations. Understanding these hurdles and choosing the right partner is essential for successful, sustainable AI deployment.
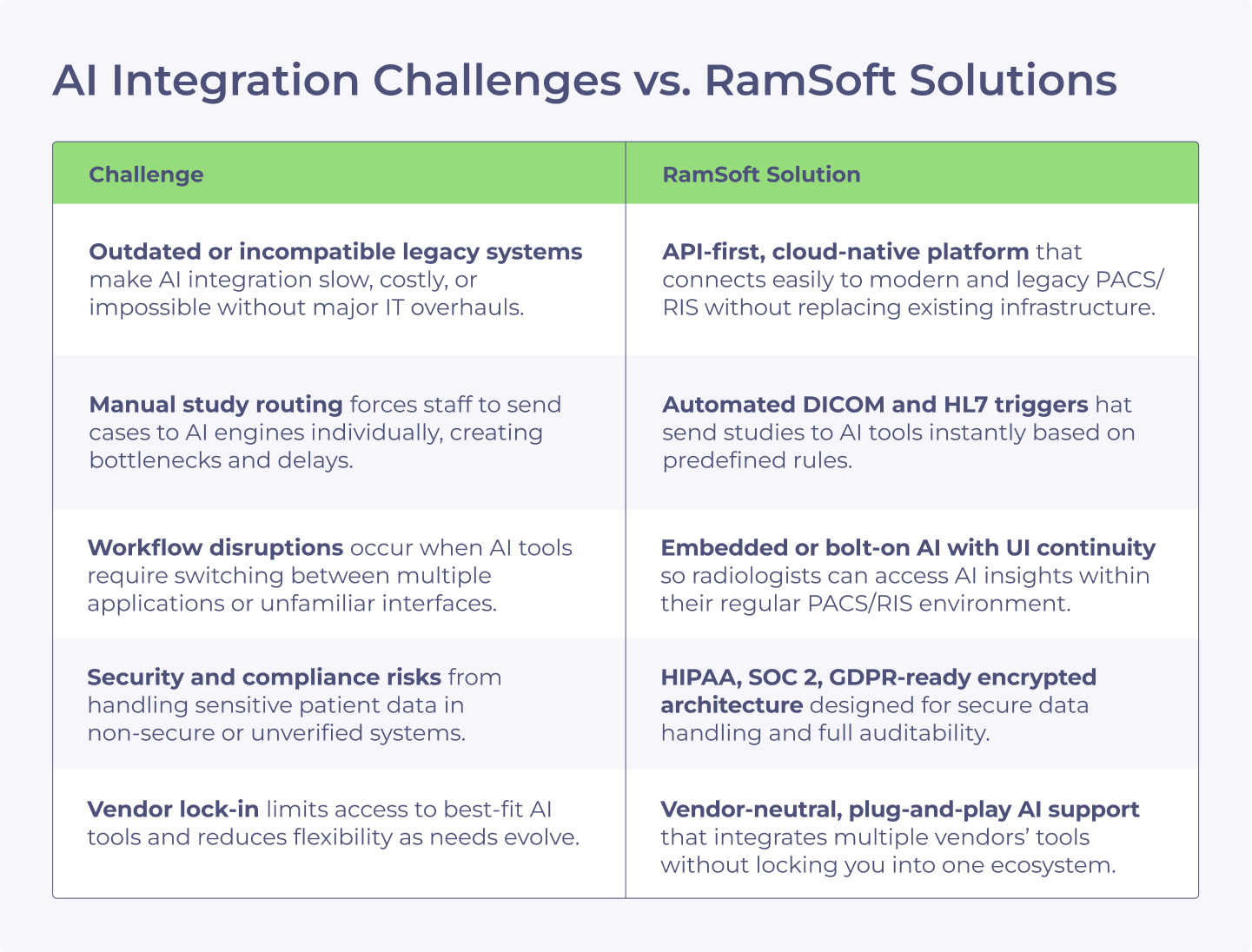
Compatibility with Existing Infrastructure
One of the primary challenges lies in connecting new AI solutions to existing PACS and RIS systems, many of which were designed years ago and lack modern interfaces. Legacy software and hardware can make integration complex, requiring custom development, middleware, or costly system upgrades.
Radiology departments often operate with mixed environments where some modalities or archives remain on-premises, while others have moved to the cloud. This disparity complicates consistent AI deployment across the enterprise.
Cloud-ready and API-driven architectures are increasingly crucial for overcoming these hurdles. Solutions like RamSoft’s cloud-native platforms are built to integrate seamlessly with AI applications via standardized APIs, reducing reliance on proprietary interfaces and enabling future scalability.
For practices seeking to modernize, transitioning to systems designed for interoperability and vendor-neutral connectivity is a critical step toward integrating advanced AI workflows without disrupting core operations.
Data Quality and Standardization
AI performance depends on the quality of the data it analyzes. Radiology departments frequently encounter challenges with inconsistent metadata, variations in imaging protocols, and differences in annotation formats across institutions and equipment vendors. Even minor inconsistencies in DICOM tags can lead to errors in AI algorithms, compromising diagnostic accuracy.
Structured, standardized data is essential to enable AI systems to learn effectively and perform reliably. Clean datasets ensure that AI tools can detect subtle patterns without confusion from data irregularities. Practices implementing AI must prioritize consistent data labeling, adhere to established protocols, and leverage tools that support harmonization across different imaging sources.
RamSoft’s products support standardized data management and interoperability through DICOM, HL7, and FHIR, helping ensure AI solutions receive the quality input they require for high performance.
Clinical Workflow Disruptions
Integrating AI into radiology should simplify workflows, not create unnecessary friction. Yet one of the most common barriers to adoption is disruption to established processes. Radiologists are under constant pressure to deliver fast, accurate results. If AI tools require excessive switching between applications, add too many extra clicks, or demand manual data entry, they risk slowing down processes instead of improving them.
The key to overcoming this challenge is seamless integration into existing clinical tools and user interfaces. Well-designed AI systems embed their results directly into the radiologist’s PACS viewer or reporting environment, maintaining familiar workflows while delivering new insights. User interface design is equally important; AI outputs must be intuitive, clear, and actionable without overwhelming radiologists with excessive data or alerts. Automation plays a vital role in minimizing manual steps, ensuring AI augments radiologists’ work rather than complicating it.
AI widgets are becoming a preferred method for presenting AI findings. These can be turned on or off at any point in the workflow, allowing radiologists to review AI insights as a second opinion without introducing bias during the initial read. This approach promotes independent decision-making, prevents overreliance, and positions AI as an on-demand aid rather than a constant influence.
Regulatory and Privacy Concerns
AI in healthcare operates under strict regulatory scrutiny to protect patient safety and data privacy. Systems deployed in clinical practice must comply with standards such as HIPAA in the United States, GDPR in Europe, and local data protection laws in other regions. This means patient data used to train or run AI algorithms must be de-identified, stored securely, and managed with clear consent protocols.
Equally important is regulatory approval for AI tools themselves. Solutions intended for diagnostic use often require FDA clearance or similar certifications in other jurisdictions. Developers must demonstrate clinical safety, effectiveness, and transparency in how algorithms make decisions. Practices considering AI integration should demand documentation of regulatory compliance and understand how vendors address privacy concerns.
RamSoft’s platforms are built with robust security, encryption, and audit trails to support compliance and protect patient data. As AI becomes more central to diagnostic workflows, ensuring regulatory alignment will be critical for safe, ethical, and trusted deployment.
Technical Challenges in AI Integration
Alongside operational considerations, technical challenges can pose significant obstacles to successfully integrating AI into radiology environments. Practices must assess infrastructure readiness, system performance, and ongoing maintenance needs to ensure AI solutions deliver value without disruption.
Interoperability and Standards
AI solutions must communicate effectively with diverse systems across the imaging ecosystem. Standards like DICOM, HL7, and FHIR ensure structured data exchange, enabling AI algorithms to receive and send information seamlessly. However, differences in implementation among vendors can create compatibility issues, requiring custom interfaces or middleware.
RamSoft’s cloud-native architecture prioritizes interoperability through API-driven design and support for industry standards. This approach helps ensure that AI integrations remain vendor-neutral and sustainable as technology evolves.
Compute and Storage Requirements
AI tools analyzing high-resolution imaging data demand significant computing power and storage. On-premises infrastructure often struggles to meet these needs.
RamSoft solves this with cloud-native solutions powered by Microsoft Azure. Practices can run advanced AI workflows without costly hardware, scaling resources as imaging volumes grow. Azure ensures fast performance, secure data handling, and compliance with standards like HIPAA and SOC 2.
Model Lifecycle Management
AI models must be continuously monitored, updated, and validated to maintain clinical sensitivity and effectiveness. Practices need monitoring processes for managing model versioning, tracking performance metrics, and ensuring regulatory compliance over time. Without proper oversight, even high-performing AI systems can drift in accuracy due to changing data distributions or evolving clinical standards.
Strategies for Successful AI Integration with RIS/PACS
While the benefits of AI in radiology are substantial, achieving a smooth and impactful integration requires deliberate planning and ongoing management. Radiology practices that approach AI deployment strategically can minimize risks, control costs, and ensure that new tools deliver measurable improvements in detection, speed, consistency, and patient care. Below are key strategies for implementing AI successfully into RIS and PACS environments.
Start with High-Impact Use Cases
Implementing AI works best when it begins with focused, high-value applications rather than attempting to overhaul entire workflows immediately. Radiology practices should prioritize use cases that deliver clear, measurable benefits, such as AI-driven triage for critical findings like pulmonary embolism or stroke.
Starting with narrow, high-ROI tasks allows teams to demonstrate value quickly, secure clinician buy-in, and reduce the complexity of early integration. Successful pilot projects create momentum and provide a framework for expanding AI adoption into broader applications across the enterprise.
Validate AI Performance Locally
AI tools may perform well in vendor tests or published studies, but real-world accuracy can vary based on patient demographics, imaging protocols, and equipment differences. Before widespread deployment, practices should rigorously validate AI solutions using internal data and representative case samples.
Local benchmarking ensures that AI tools meet clinical expectations and adapt effectively to the specific environment in which they’ll operate. By conducting thorough evaluations upfront, radiology teams can identify performance gaps, calibrate thresholds, and reduce the risk of errors in live clinical workflows.
Ensure End-to-End Visibility
AI solutions need to offer full traceability of decisions and actions. Radiology practices should implement systems that log every AI prediction, flag, or measurement, creating an auditable trail for compliance, troubleshooting, and performance review.
Detailed logging helps detect unusual algorithm behavior, facilitates root-cause analysis when discrepancies occur, and supports regulatory requirements such as those under HIPAA or the FDA for medical devices. End-to-end visibility builds confidence among clinicians and ensures that AI tools can be integrated safely and reliably into critical patient care processes.
Involve Radiologists Early
AI projects thrive when radiologists are engaged from the beginning. Their insights are crucial for defining meaningful use cases, selecting relevant performance metrics, and shaping workflows that integrate AI seamlessly into daily practice. Involving radiologists during pilot phases ensures the tools are usable, clinically relevant, and tailored to real-world reading environments.
Regular feedback sessions help refine user interfaces, reporting outputs, and alert mechanisms, ensuring that AI enhances rather than disrupts clinical productivity. Radiologists’ early involvement fosters trust in new technologies and increases adoption rates across the department.
Monitor and Tune Continuously
AI integration is ongoing oversight and adjustment. Radiology teams should establish processes for continuously monitoring AI performance, including reviewing logs, tracking false positives or negatives, and identifying edge cases where the algorithms may struggle.
Routine audits and performance reviews help keep AI tools aligned with evolving clinical standards, new disease patterns, or changing imaging protocols. Thresholds may need periodic adjustments to maintain sensitivity and specificity. Proactive tuning ensures that AI continues delivering high-quality results and remains a valuable asset rather than a source of workflow friction or diagnostic risk.
By following these strategies, radiology practices can move beyond simply acquiring AI tools to achieving meaningful integration that supports faster diagnoses, greater accuracy, and improved patient outcomes. RamSoft’s experience with cloud-native architecture and vendor-neutral integration equips practices to navigate these steps successfully, ensuring AI becomes a reliable, transformative part of everyday radiology operations.
How RamSoft Cloud Architecture Supports AI Integration
RamSoft’s cloud architecture is designed to make AI integration seamless, scalable, and secure for radiology practices. Traditional on-premises solutions often require complex configurations or additional middleware, but RamSoft’s platforms are built to connect with AI tools without disrupting existing workflows. By combining an API first approach, vendor neutral interoperability, and enterprise grade security, RamSoft enables radiology teams to leverage AI with minimal IT overhead.
API First Design
RamSoft systems use modern RESTful APIs that simplify integration with third party AI tools. These APIs allow imaging data, annotations, and structured reports to flow directly between PACS and RIS and external AI engines without manual routing or file conversions.
Developers can easily connect AI algorithms for tasks such as lesion detection, segmentation, or triage using standardized endpoints. This reduces integration timelines, eliminates reliance on custom interfaces, and ensures that AI outputs are available within the same environment where radiologists review studies, improving efficiency and usability.
Cloud Native Scalability
AI powered imaging tasks such as analyzing thousands of high resolution CT or MRI slices require significant compute and storage capacity. RamSoft’s OmegaAI cloud native infrastructure scales automatically to handle heavy AI workloads without slowing down performance.
Radiology practices avoid the cost and complexity of upgrading local hardware, as compute intensive processes are distributed across secure cloud resources. This scalability is especially valuable for practices experiencing fluctuating imaging volumes or expanding to new AI driven services, ensuring consistent performance during peak demand.
Vendor Neutral AI Support
RamSoft takes a plug and play approach to AI, allowing practices to choose the best tools for each modality or clinical application. Whether connecting with platforms like iCAD and Therapixel for AI-CAD in mammography, RamSoft’s vendor neutral design avoids locking customers into a single ecosystem. This flexibility allows radiology teams to adopt specialty specific tools and integrate multiple AI vendors within the same workflow while maintaining a unified user experience.
Real Time Integration
AI insights are most effective when delivered directly into clinical workflows. RamSoft supports real time integration by returning AI outputs such as annotations, probability scores, or flagged findings into radiologists’ worklists and reporting tools through DICOM and HL7.
For some partners like CARPL, results can be viewed directly within the PowerServer™ interface. For others, bolt-on integrations may launch AI viewers or widgets with minimal disruption. By reducing manual steps and enabling timely access to insights, these integrations help radiologists make faster, more confident decisions.
Security and Compliance
Data security is a core part of RamSoft’s cloud architecture. All AI data exchanges occur through encrypted pipelines, and every action is logged for auditability and compliance. RamSoft adheres to strict standards including HIPAA, GDPR, SOC 2 Type II, and PIPEDA, ensuring that sensitive imaging data remains protected throughout the AI workflow.
Role-based access controls and automated audit trails add an extra layer of security, giving radiology practices confidence that AI integrations meet both regulatory requirements and internal data governance policies.
The Future of AI Integration in Radiology Workflows
AI in radiology is moving beyond detection and reporting to become an active driver of intelligent automation across the imaging ecosystem. One emerging trend is RIS-driven automation, where AI assists with scheduling, coding, and administrative tasks. This not only reduces manual effort but also ensures faster billing cycles and improved operational efficiency.
Another advancement is adaptive AI that learns from radiologist behavior over time. These systems can adjust thresholds, prioritize studies based on individual preferences, and provide personalized decision support. By aligning with the unique reading patterns of each radiologist, AI can further improve workflow efficiency and accuracy.
Federated learning is also gaining momentum. Instead of sharing sensitive patient data across institutions, AI models are trained locally and updated collaboratively. This approach protects patient privacy while creating models that are robust and generalizable across diverse populations.
Finally, interoperability standards such as DICOM AI and FHIR AI are becoming essential for seamless integration. These frameworks ensure that AI-generated insights can be exchanged across platforms, supporting a future where AI is deeply embedded in every stage of the radiology workflow.
Frequently Asked Questions
How does AI integration improve RIS workflows?
AI streamlines RIS workflows by automating scheduling, coding, eligibility, prior authorization, digital fax management, and follow-up tasks. It reduces manual effort, improves data accuracy, and ensures faster case handling. Integrated AI helps radiologists and staff focus on clinical care rather than administrative steps, enhancing efficiency across the imaging workflow.
Can AI tools be integrated with both PACS and RIS simultaneously?
Yes, AI tools can integrate with both PACS and RIS. Imaging data flows through PACS, while structured results and study updates return to RIS. This dual integration ensures clinical and administrative teams access the same AI insights, improving coordination and workflow consistency.
How does AI affect radiology?
AI improves radiology by speeding up image interpretation, reducing errors, and managing high imaging volumes. It detects abnormalities, automates measurements, and prioritizes urgent cases. This helps radiologists work faster and make more accurate decisions for better patient care.
How does AI integration enhance patient care in radiology?
AI speeds up critical diagnoses, reduces delays, and ensures consistent, high-quality reporting. By embedding AI into daily workflows, radiologists can prioritize urgent cases and deliver faster results. Acting as a second reader, AI adds another layer of review, helping improve accuracy and patient safety.
What is the best approach to integrate AI into RIS?
Start with focused use cases like coding or structured reporting. Validate performance on local data and work with vendors offering open APIs and HL7 support. Choose a RIS platform, like RamSoft’s, that supports scalable, seamless AI connections with minimal disruption.














